How Dod You Calculate The Gross Death Rate For The Surgical Service
Statistics and data presentation
Valerie J.One thousand. Watzlaf and Elaine Rubinstein
Objectives
• Compute health care statistics, including mortality and morbidity rates, autopsy rates, measures of central tendency, and dispersion, and determine the most appropriate use of these health care statistics in wellness information management.
• Organize data generated from wellness care statistics into appropriate categories, including nominal, ordinal, discrete, and continuous.
• Display information generated from health care statistics using the most advisable tables, graphs, and figures, including frequency tables, bar graphs, histograms, Pareto diagrams, pie charts, and frequency polygons.
• Determine which tests of significance should be used to examination specific hypotheses and which are most appropriate for certain types of information.
Central words
Alternative hypothesis
Anesthesia death charge per unit
Dissection rate
Average daily inpatient demography
Average length of stay
Bar graph
Bed turnover charge per unit
Census statistics
Coefficient of variation
Community-acquired infection
Comorbidity
Confidence interval
Contingency table
Continuous data
Straight method of age aligning
Detached information
Dispersion
Fetal death charge per unit
Frequency distribution
Frequency polygon
Gross decease rate
Histogram
Hypothesis
Incidence
Incidence rate
Baby decease rate
Infer
Inpatient bed occupancy rate
Interval data
Length of stay
Level of significance
Maternal death charge per unit
Mean
Median
Mode
Morbidity rates
Mortality rates
Neonatal expiry rate
Net death charge per unit
Nominal information
Nosocomial infection
Nix hypothesis
Ordinal information
p value
Pearson correlation coefficient
Percentage
Percentage of occupancy
Pie chart
Postoperative death charge per unit
Postoperative infection rate
Prevalence
Prevalence rate
Proportion
Random sample
Range
Rate
Ratio
Ratio data
Regression analysis
Sampling error
Standard deviation
Standardized mortality ratio
Stratified random sample
Systematic sampling
Exam statistic
Tests of significance
Variance
Vital statistics
Weighted mean
Abbreviations
AIDS—Caused Immunodeficiency Syndrome
ALOS—Average Length of Stay
ANOVA—Analysis of Variance
CV—Coefficient of Variation
dfb—Degrees of Freedom, Between Groups
dfw—Degrees of Freedom, Inside Groups
DRG—Diagnosis-Related Group
HIM—Health Information Direction
ICD— International Classification of Diseases
MSB—Hateful Square Betwixt Groups
MSW—Hateful Square Inside Groups
NCHS—National Centre for Wellness Statistics
SMR—Standardized Mortality Ratio
SSB—Sum of Squares Betwixt Groups
SSW—Sum of Squares Inside Groups
Pupil Study Guide activities for this chapter are bachelor on the Evolve Learning Resources site for this textbook. Please visit evolve.elsevier.com/Abdelhak.
When yous see the Evolve logo  , go to the Evolve site and consummate the corresponding activity, referenced by the page number in the text where the logo appears.
, go to the Evolve site and consummate the corresponding activity, referenced by the page number in the text where the logo appears.
Overview of statistics and information presentation
Wellness care organizations continuously generate health care data. These data are used internally by patients, medical staff, nursing staff, and physical, occupational, and speech communication therapists and externally by state and federal regulatory agencies, the Joint Commission, and insurance companies, to name but a few. No affair who the user may be, statistics and data presentation focus on answering the user's questions while complying with the standards of the wellness care facility. To accomplish this goal, various methods are used to calculate specific types of statistics. Different rates, ratios, proportions, and percentages are used to evaluate mortality, autopsy, and morbidity rates and demography and vital statistics.
Organizing and displaying health intendance data are necessary. To choose appropriate methods of displaying and analyzing data, the health information management (HIM) professional must identify the level of measurement (nominal, ordinal, interval, or ratio) for variables and determine whether data are continuous or discrete. Measures of central tendency (mean, median, mode) and dispersion (variance and standard divergence) and tests of significance are used to describe and analyze data. It is as well important for the HIM professional to understand bones principles of sample size conclusion and to be familiar with normally used statistical tests such every bit analysis of variance (ANOVA), correlation, and regression.
This chapter explains bones and avant-garde health care statistics that are used in the health care field. Each statistic is defined and the formula for calculating each statistic is provided along with examples of how each statistic is used. Various methods of displaying data are described and illustrated.
Role of the health information management professional
Now more ever, health care data are being collected to serve many purposes. One primary purpose is to establish health care statistics to compare trends in incidence of disease, quality and outcomes of care, and management of wellness information departments; another primary purpose is to bear epidemiological research. The HIM professional'southward goal is to collect, organize, display, and interpret health care information properly to meet the needs of the users. Data tin exist manipulated in many ways to demonstrate one consequence or some other. HIM professionals need a broad base of operations of cognition to determine which information elements should exist used and when data are beingness analyzed appropriately or inappropriately. To practice this, an understanding of health care and vital and public health statistics is necessary. Furthermore, knowledge of statistical analysis is necessary then that HIM professionals can be the forerunners in data analysis. Because HIM professionals oversee a vast array of health data, it is imperative that the interpretation of the analysis and results of wellness care information start with them.
The HIM professional should presume the lead in recommending and using statistical tests that promote improvement in the analysis, apply, and dissemination of health intendance data. The HIM professional fills many diversified roles and responsibilities, such as clinical vocabulary manager, information miner, or clinical trials manager.
In each of these roles, understanding and applying the methods used to collect, analyze, display, interpret, and disseminate information are essential. Responsibilities undertaken in these roles may vary from person to person. For example, the clinical trials manager may play a clearly visible function in cancer enquiry study analysis and estimation of the data, the clinical vocabulary manager may play a key role in developing vocabularies and standards that tin can be effectively used in the design of the electronic health tape, and the data miner may make up one's mind the appropriate databases to employ when analyzing clinical and financial data.
The HIM professional may presume other managerial roles in which statistics are used to assess productivity in coding, transcription, correspondence, and record analysis. The HIM professional should have sufficient cognition and skills to do the following:
Health intendance statistics
Vital statistics
Vital statistics include data collected for vital events in our lives, such as births and adoptions, marriages and divorces, and deaths, including fetal deaths. Birth, death, and fetal decease certificates are familiar reports to HIM professionals. Although each state can determine the format and content of its certificates, the National Eye for Health Statistics (NCHS) recommends standard forms that most states have adopted. The purpose of the NCHS standard forms is to have a national uniform reporting system of vital statistics. These standard forms are revised periodically. The attending physician is responsible for the completion of nascency, death, and fetal decease certificates. The authentic completion of these certificates is supervised by the HIM department, and a copy of the birth or decease certificate is kept in the medical record. A copy of the fetal death certificate is kept in the mother's medical record.
When the certificate is complete, the original is sent to the local registrar, who keeps a copy and forwards the original to the state registrar. At each of these stages, the certificate is checked by the registrar to brand sure it is complete. Individuals tin obtain from the state registrar certified copies of birth, death, and fetal death certificates. Each state sends electronic files of nativity and decease statistics to the NCHS. The death statistics are so compiled in the National Death Index. The Death Alphabetize is a central computerized index of death tape information used for research purposes by epidemiologists and other workers involved in health care research.i The natality, or nascency, statistics are compiled in the monthly vital statistics reports, and the data files are likewise available for purposes of research.
Refer to your country wellness data eye or division of vital statistics to receive state-specific information on preparing and registering vital records.
Rates, ratios, proportions, and percentages
A rate is defined as the number of individuals with a specific characteristic divided past the total number of individuals or, alternatively, as the number of times an upshot did occur compared with the number of times information technology could take occurred.
A rate contains ii major elements: a numerator and a denominator. The numerator is the number of times an issue did occur. The number of events under study, or the numerator alone, conveys piffling information. Nonetheless, when the numerator is compared with the denominator or the population of people in which the event could have occurred, a rate is determined. The results of a quality improvement study showed that 20 patients with diabetes had a stroke while taking a certain medication. What does this tell y'all? Should this medication be discontinued in this population? The data provided here include simply the numerator. To compute a rate, the denominator is needed—for this example, total number of patients with diabetes who are taking the medication. This particular example included a sample size of 1000 patients. The rate is xx in 1000 or ii in 100. A rate is usually expressed in the following manner: 20 in yard, two in 100, 1 in 100,000, 10 in 1,000,000, and then on.
However, rates are too ordinarily expressed every bit percentages past converting the rate into a decimal and so multiplying the decimal by 100. A percentage is based on a whole divided into 100 parts. In the preceding example, the rate could too be expressed as a percentage by taking 20/1000 = 0.02 × 100 = 2% or past taking 2/100 = 0.02 × 100 = two%. This tells united states that 2% of the patients with diabetes (in the written report) had a stroke while taking a certain medication. To express a fraction, such as ⅕, equally a percentage, the starting time stride is converting the fraction into a decimal past dividing the numerator, 1, by the denominator, v, to obtain 0.20. The decimal is and so converted into a percentage past multiplying the decimal by 100, which tin can be achieved by moving the decimal betoken two places to the right. The result of this process is 20%.
A proportion and a ratio are similar to a rate. A proportion, which is a part considered in relation to the whole, is normally expressed as a fraction—20/g, two/100, 1/100,000, 10/i,000,000, and so on. A ratio is a comparing of ane matter to another, such as births to deaths or marriages to divorces. A ratio is expressed as 20:1000, 2:100, one:100,000, ten:ane,000,000, and so on. The number of physicians relative to patients or teachers relative to students is normally expressed as a ratio. For instance, if a physician group practise has ten physicians and grand patients, the ratio is 10:yard, which reduces to 1:100.
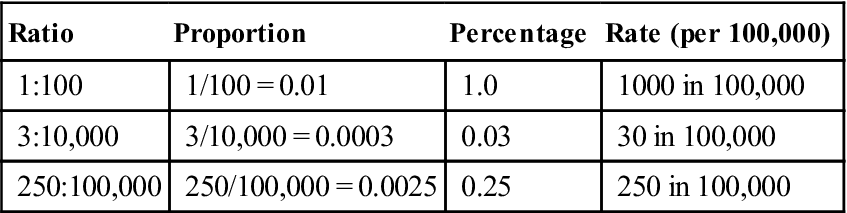
Table ten-i summarizes examples of rates, proportions, ratios, and percentages.2 , 3
Table 10-one
EXAMPLES OF RATIOS, PROPORTIONS, PERCENTAGES, AND RATES
| Ratio | Proportion | Percentage | Rate (per 100,000) |
| 1:100 | ane/100 = 0.01 | 1.0 | 1000 in 100,000 |
| 3:10,000 | 3/10,000 = 0.0003 | 0.03 | 30 in 100,000 |
| 250:100,000 | 250/100,000 = 0.0025 | 0.25 | 250 in 100,000 |
Once percentages are calculated, they can be compared across different subgroups, as seen in Tabular array 10-2. This table concisely shows differences amongst geographic areas in the percentage of elderly people past age categories. It fifty-fifty allows a glance toward the futurity by projecting percentages for the years 2010 and 2025. Comparing percentages among areas shows that Europe has the highest percentage of population aged 65 years or older (13.vii% in 1990) and that it should remain the world leader for at least the side by side 3 decades. Due north America and Oceania too have relatively high percentages of elderly people, which are projected to increase substantially from 1990 to 2025.iv
Bloodshed rates
Mortality rates are computed because they demonstrate an outcome that may be related to the quality of the wellness care provided. At that place are many types of bloodshed rates. Table x-3 provides definitions and formulas for the most commonly used mortality rates.two , iii
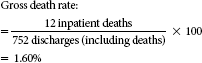
Gross death rate
The gross death rate is a crude death rate for infirmary inpatients because it does not consider such factors as age, gender, race, and severity of illness, which also play an important part in death rates. The use of the gross death charge per unit as a mensurate of quality in health care has been questioned because it does not take these factors into account. As long every bit the HIM professional is aware that other factors influence this rate and that they have non been taken into account in the calculation, the gross death rate can be a quick, useful ways of analyzing mortality in hospital inpatients (see the following instance of gross death rate).
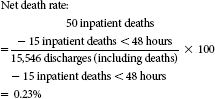
Cyberspace death rate
The net death rate is different from the gross decease rate considering information technology does non include deaths that occurred less than 48 hours afterwards access to the health care facility. The internet decease charge per unit is useful because information technology provides a more realistic account of patient deaths related to patient intendance provided past a specific wellness care facility. For example, a 90-year-one-time patient arrives at the emergency department with shortness of breath, chest pain, and arrhythmia. After being evaluated, the patient is admitted, and it is determined that he has had a severe myocardial infarction (see the example of cyberspace death rate).
Approximately 24 hours afterwards, the patient has cardiac arrest and dies. This item death would exist included in the gross death rate but non the cyberspace death charge per unit because it occurred less than 48 hours after admission. Reporting agencies sometimes request net expiry rates because they may provide a more realistic reflection of patient care provided than gross death rates do. Nonetheless, internet decease rates still practice non have into consideration other chance factors that may also affect decease, such as age, gender, race, and then forth. Therefore, an important note is that health intendance facilities are not necessarily responsible for deaths that occur more 48 hours after patients are admitted; on the other hand, health care facilities are not necessarily free of responsibleness for deaths that occur inside 48 hours of admission. For this reason, some health care facilities do not make apply of or report the net expiry charge per unit.
Some other consideration when calculating any mortality rate is a health care facility must decide whether newborn inpatients will be included in these calculations. This decision is upwards to the wellness intendance facility; however, if a facility decides that newborn inpatient deaths will be included in the numerator, all newborn discharges must also be included in the denominator.
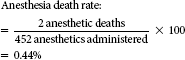
Anesthesia decease rate
The anesthesia death charge per unit can besides exist referred to as a cause-specific death rate because the expiry is adamant by a physician or medical examiner to be due to a specific cause (e.thou., an anesthetic agent). This rate indicates the number of deaths that are due to the administration of anesthetics for a specified menstruum of time. If the contempo anesthetic death rate is college than the rate in previous periods, a focused evaluation may be necessary to determine why this is so (encounter the example of anesthesia expiry rate).
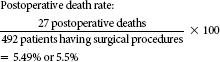
Postoperative decease rate
The postoperative death rate may be considered a crusade-specific death charge per unit as well. This death rate indicates the number of patients who dice within ten days of surgery divided past the number of patients who underwent surgery for the period; therefore, information technology expresses the number of deaths that may have resulted from surgical complications. In both the anesthesia and the postoperative death rates, other risk factors, such equally age, gender, race, and severity of illness, are not considered. Therefore, if information technology is institute that these rates are college in certain periods than in others, specific evaluations are necessary to determine whether the increase is truly due to the anesthesia or surgery or to other take chances factors (see the example of postoperative death charge per unit).
Maternal death rate
Death rates are further categorized according to the type of service or section, such equally the maternal bloodshed or death rate. A maternal death results from causes associated with pregnancy or its management merely not from accidental or incidental causes unrelated to the pregnancy. The maternal expiry rate is the number of maternal deaths divided past the number of obstetric discharges. Again, similar all the rates described previously, the maternal death rate does non take into business relationship any other risk factors. The maternal death rate is useful because maternal deaths are rare. Therefore, if there is even one maternal death in a period, it is necessary to examine the cause of death in more detail (meet the instance of maternal expiry charge per unit).
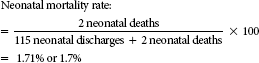
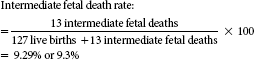
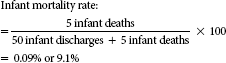
Neonatal, babe, and fetal death rates
The formulas for these rates are given in Table ten-3. Neonatal and baby death rates are computed to examine deaths of the neonate and infant at dissimilar stages. A neonatal expiry is the death of an babe within the first 27 days, 23 hours, and 59 minutes of life. An infant decease is death of an infant at any time from the moment of nativity through the first year of life. Both of these figures are compared with the number of neonates and infants, respectively, who were discharged and died during the aforementioned flow.
Fetal decease rates are computed to examine differences in the rates of early, intermediate, and late fetal deaths. The definition of early, intermediate, and late fetal deaths may vary from state to country. These deaths are distinguished by the length of gestation or the weight of the fetus.
Encounter the example of neonatal, infant, and fetal death rates.
Using and examining bloodshed rates
Mortality statistics and trends are analyzed and used in many ways. When trends in mortality are examined, the possible reasons for differences in mortality rates should be considered. The influences can be grouped into three variables: time, identify, and person. Changes over fourth dimension include the following:
Finally, the following characteristics of groups of people can also influence mortality:
All these factors must be taken into consideration when mortality trends are examined within the health intendance facility or beyond health care facilities in relation to the quality of care provided.v
When examining mortality rates inside a specific population equally in the gross and cyberspace death rates, it is important to testify age-specific rates or to adapt for age. Mortality rates are routinely adapted for age because it is the most important influence in relation to death. As a person ages, the likelihood that the person will die increases. Historic period-specific rates can be used, only it becomes hard to brand comparisons of data with four or more than age levels or categories. Therefore, age adjustment is performed. Statistically, age aligning removes the difference in composition with respect to historic period.i
Ii methods can be used to perform age aligning. Ane is the direct method of age aligning, and the other is the indirect method of age adjustment or standardized mortality ratio (SMR). The calculations for these 2 methods are shown in Table 10-4.
The direct method uses a standard population and applies the age-specific rates available for each population. The expected number of deaths in the standard population is then determined. To use the direct method of age adjustment, historic period-specific rates must be available for both populations and the number of deaths per age category should be at least v. The indirect method, or SMR, is used more than oft and can be used without age-specific rates and when the number of deaths per age category is small or fewer than five. Standard rates are so applied to the populations beingness compared to calculate the expected number of deaths, which is compared with the observed number of deaths.6
Considering the SMR is used in nearly national and statewide bloodshed reports, it is explained in more than item here. For instance, in Tabular array 10-5, hospitals across a land are examined for expiry rates associated with the diagnosis-related group (DRG) 127—Eye Failure and Daze.
The bodily or observed number of deaths in the hospital is compared with the expected number of deaths. The expected number of deaths is taken from a comparative national database adjusted for age and patient severity for each DRG. Table 10-5 shows a sample of the hospitals that treated patients included in DRG 127 and the actual and expected number of deaths. An SMR of 1 means that the number of observed deaths and the number of expected deaths are equal, and therefore the mortality rate is equal to what is expected from national norms. An SMR less than ane means that the observed deaths are lower than the expected deaths, and therefore the mortality rate is lower than expected from national norms. An SMR of greater than one means that the observed deaths are greater than the expected deaths, and therefore the mortality rate is higher than expected from national norms (run across the examples of use of SMR).
Autopsy rates
Autopsy rates are computed so that the health care facility can determine the proportion of deaths in which an autopsy was performed. This enables the facility to examine why a higher or lower autopsy rate may be seen from i calendar month to another. Autopsies are performed to determine the crusade of decease, to better empathize the affliction process, or to collect tissue samples, as in patients with Alzheimer'south disease. Autopsy rates can be further broken down to bear witness the gross autopsy rate, or the rate of autopsies performed for total inpatient deaths; the net autopsy charge per unit, or the rate of autopsies performed for inpatient deaths, excluding unautopsied coroner cases; and the adjusted hospital autopsy rate or the autopsy rate performed for all deaths of infirmary patients whose bodies are bachelor or brought to the hospital for autopsy (those non removed past coroners, medical examiners, and so on). Autopsies may be performed after the deaths of inpatients, outpatients, home care patients, skilled nursing intendance residents, patients who died at home, previous patients, and and then on (meet case of hospital autopsy rates). Table 10-6 presents the about commonly used autopsy rates.3
Morbidity rates
Morbidity rates can include complication rates, such as community-acquired, hospital-acquired or nosocomial, and postoperative infection rates. They can also include comorbidity rates and the prevalence and incidence rates of disease.
Hospitals use each of these rates to report the types of disease or conditions that are nowadays within the health care facility and to examine the quality of care provided past the facility. These rates tin assist health care facilities in planning specific health intendance services and programs. Table 10-seven provides a summary of the more than common morbidity rates and the formulas used to compute them.iii
Complications include infections, allergic reactions to medications, transfusion reactions, decubitus ulcers, falls, burns, and errors of medication administration. The complication rates for any of these complications can also be computed by using the formula for complication rates listed in Tabular array 10-seven.
One of the virtually common complications is infections. Infection rates are computed so that the health care facility tin determine when infections developed and, therefore, how they may be prevented. A nosocomial, or facility-acquired, infection rate includes infections that occur more than than 72 hours subsequently admission.7 Health care facilities may be more interested in this rate because it may show infections that occur as a consequence of the care that is provided in the facility. Further analysis of the nosocomial infection rate may show that other risk factors, such as age, compromising weather such as cancer, the use of chemotherapy treatment, and the overall severity of the affliction, may make an individual patient more susceptible to infection. Therefore, as with several of the mortality rates, other factors play a part in the development of the nosocomial infection. The postoperative infection charge per unit is commonly calculated to pinpoint how the infection may take adult. Postoperative infection rates are important to examine because the wellness care facility can determine which infections occur after surgery and are probably a result of the surgical procedure.
Distinguishing between nosocomial and community-acquired infections is important because community-acquired infections are typically present less than 72 hours earlier admission to the health care facility. Wellness care facilities may be interested in this rate because it demonstrates the infections that patients probably had earlier admission to the facility. If the facility finds that their community-caused infection rate is high, they may need to develop community-wide prevention programs, such equally administering a vaccine for pneumonia. Health care facilities can benefit from analysis of their full infection rate (both nosocomial and community-acquired infections) to determine the additional cost, length of stay, and overall issue the infections have on the quality of care provided to the patient.
Comorbidities are preexisting conditions, such as diabetes, hypertension, and osteoporosis. Analysis of the comorbidity charge per unit is important considering comorbidities can increase the length of stay and touch on the result of care provided. Comorbidities include some of the other risk factors that affect bloodshed and morbidity rates.
How Dod You Calculate The Gross Death Rate For The Surgical Service,
Source: https://nursekey.com/10-statistics-and-data-presentation/
Posted by: keyesreteneve.blogspot.com


0 Response to "How Dod You Calculate The Gross Death Rate For The Surgical Service"
Post a Comment